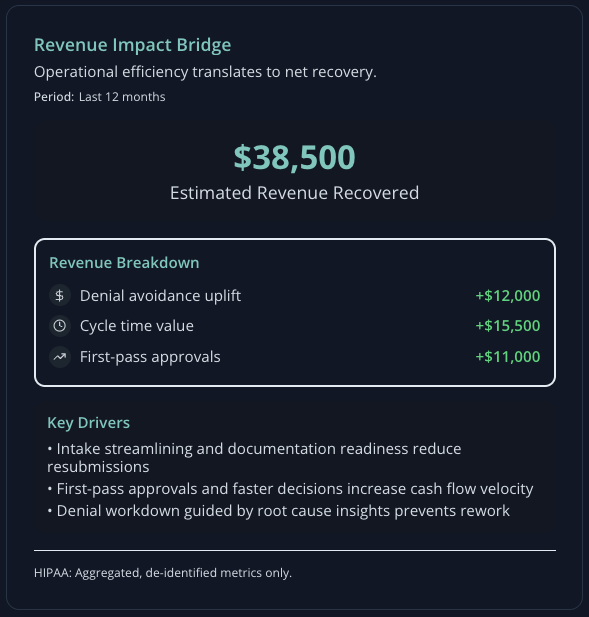
Financial gains
Fewer denials. Stronger margins.
Policy-aware submissions and payer-specific justification increase first-pass approvals and reduce write-offs.
Faster cycles. Lower DSO.
Live status, automated routing, and escalations move prior auths to decision quickly.
Less manual rework. Lower cost per auth.
Prefilled forms, missing-data checks, and payer routing reduce manual steps and increase team capacity.