The average US oncology practice devotes 16.4 staff-hours each week solely to wrangling prior authorizations, or PAs (AMA, 2024). That is nearly a full-time employee lost to copy-paste, portal logins, and status calls. Our upcoming Arkansas pilot aims to collapse those multitude of hours to just two—while also reducing denials.
read time: 5-6 minutes
The average US oncology practice devotes 16.4 staff-hours each week solely to wrangling prior authorizations, or PAs (AMA, 2024). That is nearly a full-time employee lost to copy-paste, portal logins, and status calls. Our upcoming Arkansas pilot aims to collapse those multitude of hours to just two—while also reducing denials.
A time-in-motion study found 18 distinct clicks, and three system jumps for a routine chemo request (Constant et al., 2024). Nearly half the time was spent checking prior auth status rather than entering data. Time spent chasing status updates and gathering extra information instead of entering essential clinical data takes a toll—both for patients awaiting care, but also on the mental health of clinic office staff burdened by tedious reviews.
Payers such as United Healthcare are given 72 hours to process PAs for urgent requests and up to 14 calendar days for standard requests. With the extensive amount of medical information sent to insurance case managers, each case can take more 45 minutes, meaning that fewer cases are processed and even less are approved Ultimately, less people are given the care they need especially if they have complex specialty care needs.
As one specialist told us,
“There are so many different hurdles that direct where you submit, it’s hard at times to get a hold of all of them.”
This delay is an issue seen across the country and is one heavily considered and monitored by organizations like the AMA.
Almost every specialty service and medication imaginable requires an approval request now, especially in high-cost, chronic care settings like oncology, rheumatology, and dermatology (Anderson, K. E., Darden, M., & Jain, A., 2022). Each individual prior auth form is extensive in its own way depending on the specific payer criteria, which can lead to substantial delays gathering necessary medical documents just to complete each form.
In addition to the vast amount of information and status checking that needs to be completed by clinic teams, websites and portals often time out leading to more frustration and time spent entering passwords.
Billing specialists average 35 portal logins per day, triggering password-reset tickets that cost IT teams $14 each (CAQH, 2023). With automation upgrades, logins can be drastically reduced, freeing time, boosting productivity, and approval consistency.
At the policy level, mounting pressure from lawmakers, regulators, and advocacy groups has led to significant movement on prior authorization reform. In June 2025, major insurers—including UnitedHealthcare, Cigna, and Blue Cross plans—pledged to streamline and reduce the use of prior authorizations across both commercial and government plans. These voluntary commitments include delivering real-time decisions for 80% of requests by 2027, standardizing documentation requirements, and ensuring continued coverage during insurance transitions.
When paired with automation tools, these reforms could meaningfully reduce the administrative burden clinics face. Automation not only accelerates request processing, but also ensures cleaner submissions, fewer denials, and less back-and-forth—enabling teams to act on decisions immediately and focus on delivering care.
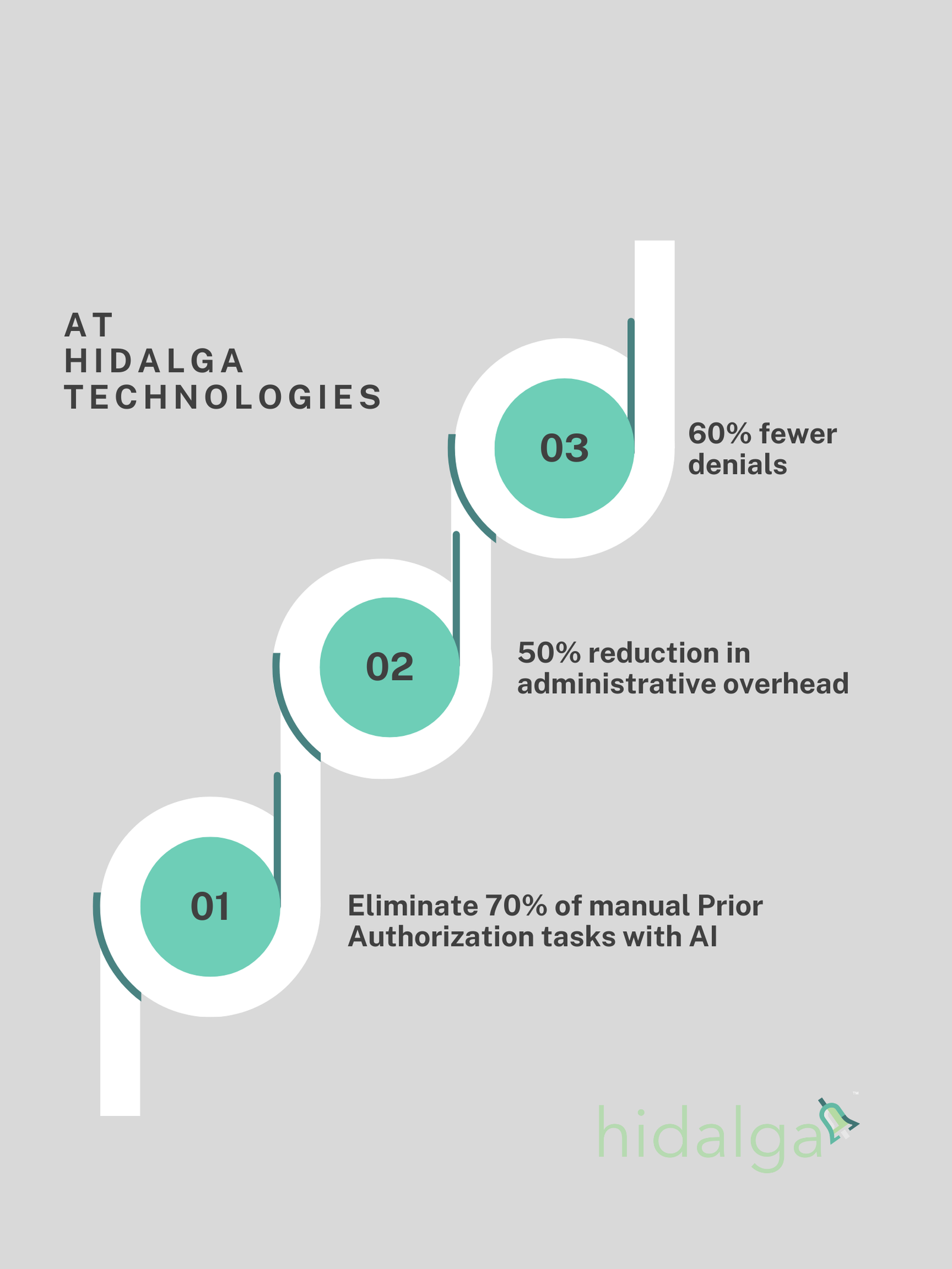
To meet these evolving needs, Hidalga Technologies is developing a software service that streamlines prior authorization submissions by optimizing workflows and eliminating repetitive portal logins. Clinics using hidalga™ can expect a 50% reduction in administrative overhead and 60% fewer denials, thanks to intelligent justification tools and automation of 70% of manual PA tasks.
By minimizing administrative friction, lowering operation costs, and supporting consistent accuracy, hidalga™ empowers practices to focus more on care and less on paperwork. With automation, clinics can reduce approval burdens, improve care timeliness, and extend their exemption status by maintaining high approval accuracy.
Clinics adopting electronic PA processes saw a 28 percent reduction in specialist turnover within 12 months (Anderson et al., 2022). By reducing the front-end burden of prior authorizations, clinics enable staff to work more efficiently and focus on patient care while at work and on self-care when off the clock. Clinic administrators know that every system comes with a price tag. But when that system is monotonous, repetitive, and prone to error, like prior authorizations, the returns from automation are clear. Imagine what your team could accomplish if they weren’t stuck in the PA queue.
Wonder how many hours your team could reclaim? Book a 15-minute workflow audit and complete a brief survey to receive a free automation time savings report.
Abelson, R. (2025, June 20). Insurers pledge to ease controversial prior approvals for medical care. The New York Times. https://www.nytimes.com/2025/06/20/health/health-insurance-prior-authorization.html
American Medical Association. (2025, April 24). Fixing prior auth: Nearly 40 prior authorizations a week is way too many. American Medical Association. https://www.ama-assn.org/practice-management/prior-authorization/fixing-prior-auth-nearly-40-prior-authorizations-week-way
Anderson, K. E., Darden, M., & Jain, A. (2022). Improving prior authorization in Medicare Advantage. JAMA, 328(15), 1497–1498. https://doi.org/10.1001/jama.2022.17732
CAQH. (2023). 2022 CAQH Index.
Constant, B. D., Albenberg, L., Mitchel, E. B., et al. (2024). Prior authorizations delay therapy… Clinical Gastroenterology and Hepatology, 22(2), 423–426. https://doi.org/10.1016/j.cgh.2023.06.021
Popatia, S., Flood, K. S., Golbari, N. M., et al. (2019). Examining the prior authorization process… Journal of the American Academy of Dermatology, 81(6), 1308–1318. https://doi.org/10.1016/j.jaad.2019.05.024
Authors:
Joshua Upshaw, PhD, Co-Founder & CEO, Hidalga Technologies, LLC
Elizabeth Grace Schmidt, MS, Software Engineer, Hidalga Technologies, LLC
This article is published by Hidalga Technologies, LLC, an Arkansas based healthcare technology company building intelligent, clinically aligned workflow optimization systems for specialty medical practices.
© 2025 Hidalga Technologies, LLC. All rights reserved.
Reproduction or redistribution of this content without written permission is prohibited. For reprint or citation inquiries, contact@hidalgatech.com.
Disclaimer: This content is intended for informational purposes only and does not constitute medical, legal, or reimbursement advice. Always consult your compliance, billing, or clinical team before making operational decisions.
You must be logged in to post a comment.